Q: I have been taking a statin and a blood pressure medication for several years now. But at a recent checkup I was told I had developed chronic kidney disease, which came as a total shock. I am 80 and have always had good health. Could my medication have caused this kidney problem?
Dr. Ellie replies: Statins and blood pressure medications are crucial drugs to reduce the risk of heart disease — but in some cases, these pills can cause other problems.
Statins reduce cholesterol, which is one of the fats in the bloodstream that can contribute to fatal heart disease or having a stroke.
Statins are not known to cause chronic kidney disease, but in rare cases the pills can trigger a condition called rhabdomyolysis, which can damage the kidneys.
One of the most common types of blood pressure medications are angiotensin receptor blockers, or ARBs, and often have an effect on the kidneys.

Statins are not known to cause chronic kidney disease, but in rare cases the pills can trigger a condition called rhabdomyolysis, which can damage the kidneys
These ARB medications relax the blood vessels by blocking the production of certain hormones in the kidneys, which helps lower blood pressure. However, this can also limit kidney function, which can sometimes lead to chronic kidney disease, where the organs slowly stop working.
However, it is important to point out that the benefits of taking these drugs almost always outweigh the risks.
High blood pressure is one of the most common causes of chronic kidney disease. This means that not taking ARB drugs is more likely to lead to kidney disease than taking them.
The medicine is even considered safe enough to be prescribed regularly to patients who already have kidney problems, albeit at a lower dose.
In addition, chronic kidney disease is a very common condition, affecting around one in five people over the age of 80.
Regardless of the cause, it is crucial that you find out the severity of your chronic kidney disease.
In the meantime, do not stop taking your other regular prescriptions unless your doctor tells you otherwise.
Q: After having a recent stroke, I developed severe pain and was prescribed daily morphine. However, it makes me feel like a zombie for hours afterwards. My doctor says that slow release morphine tablets are not currently available in the UK – is there anything else I can take instead?
Dr. Ellie replies: Unfortunately, GPs and pharmacists currently spend a lot of time dealing with drug shortages.
For a person with chronic pain, the situation is particularly serious. Pain management is an entire specialty of medicine in itself, and it can take months or even years of trying different regimens and non-pharmaceutical options to help someone through.
So it’s incredibly frustrating and debilitating to find a regimen and it’s not available here.
Also, using common opioid medications may not be the best option for pain relief.
A pain management team or pain clinic can look at all the options to help treat someone with chronic pain holistically and safely.
This would involve medication, but also psychological therapy and exercise treatments.
Consider looking beyond opioid medications for anti-inflammatory and topical treatments as well as nerve pain medications. A GP should be able to prescribe one of these alternatives as well as refer you to a pain specialist.
Q: I am a 67-year-old woman and have always had a sluggish bowel system. Last year I was diagnosed with diverticulitis. I’ve started exercising more and eating lots of fiber, but I’m still struggling with the symptoms. What should I do?
Dr. Ellie replies: Diverticular disease is an intestinal disorder that causes people to suffer on-and-off pain in the lower abdomen. It happens when small pouches form in the lower parts of the intestines called the colon.
It can cause bloating, constipation, diarrhea and most commonly abdominal pain, especially on the left side. It can also cause mucus or blood in the stool.
Increasing the amount of fiber you consume is one of the most important and effective means of combating this.
It should always be done slowly to avoid triggering possible bloating and wind.
Adults need around 30 grams of fiber a day and most of us in the UK are not eating enough, according to government figures.
Fiber in breakfast cereals or porridge is a good start, along with fruit and vegetables with skins, rye crackers, oatcakes and nuts or seeds.
Along with this, for the fiber to do its job, you need to drink two to three liters of fluid a day to help with bowel movements. Exercise also helps. Specific laxatives, called bulk-forming laxatives that contain a lot of fiber, are also used, which can help relieve the constipation or diarrhea that many patients experience.
A GP may also offer prescriptions for anti-convulsion medication to help with pain.
The charity Guts UK has excellent advice available on diverticular disease, including easy ways to increase fiber in meals. You can find out more by visiting gutscharity.org.uk.
What do you do to keep the gray at bay?
Going gray has always been considered a fact – a fate that awaits almost all of us, some sooner than others.
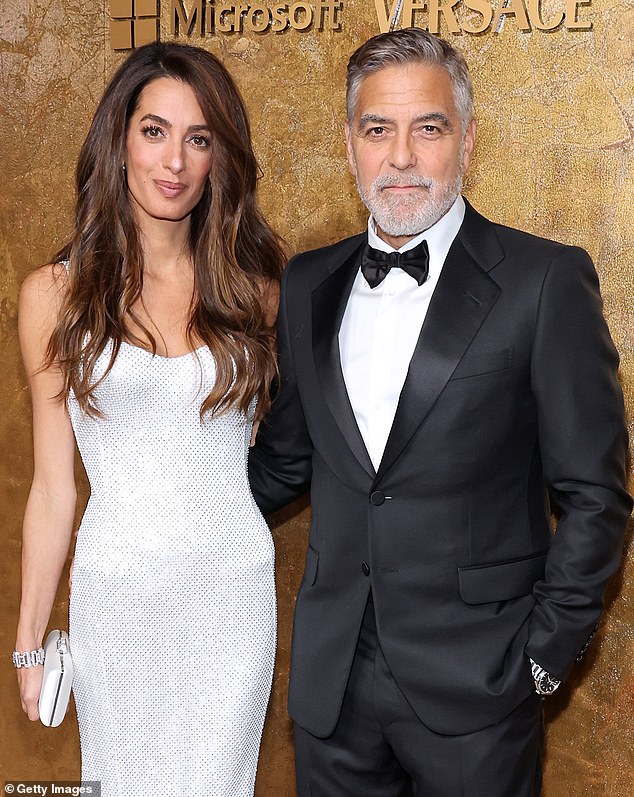
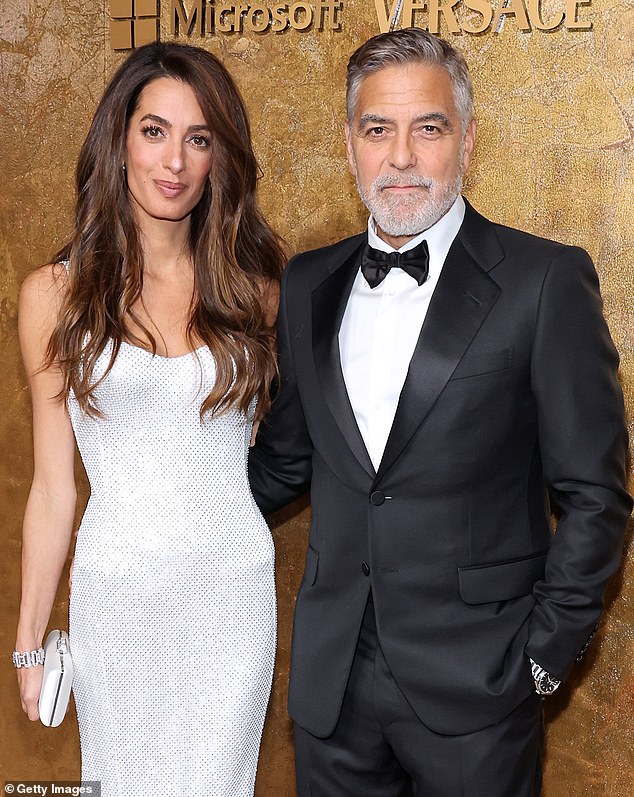
And in all my years as a GP, I have never had a patient ask if anything can be done to banish their silver locks. It has always been considered an inevitability – even for stars like George Clooney, below with wife Amal.
But while the process is largely dictated by your genes, it turns out there may be things you can do to slow down the oncoming gray hairs.
In recent years, research has found that simple steps like dealing with stress and wearing a hat in the sun can keep the gray at bay – at least for a while. So have you managed to keep your own hair color later in life and if so, what is your secret? Write to me at the email address below and let me know.
There is still cover if you are ill abroad
One of my big travel worries after the UK left the EU was the prospect of having to pay for medical treatment if someone in the family fell ill on holiday.
But I only recently discovered that while the European Health Insurance Card (EHIC) – which entitled all UK citizens to free emergency care across Europe – was scrapped after Brexit, it has been replaced by something called the UK Global Health Insurance Card ( GHIC), which offers almost identical benefits in the EU and some other countries.
If your old EHIC card has not yet expired, you can continue to use it until it does and then replace it with a GHIC, which is easy to get from the NHS website.
However, you still need travel insurance because the GHIC card does not cover the cost of medical repatriation – where you are flown home under the care of a doctor – or non-urgent treatments such as prescriptions.
Do you have a question for Dr. Ellie Cannon? Email DrEllie@mailonsunday.co.uk
Dr. Cannon cannot enter into personal correspondence and her responses should be taken in general context.
