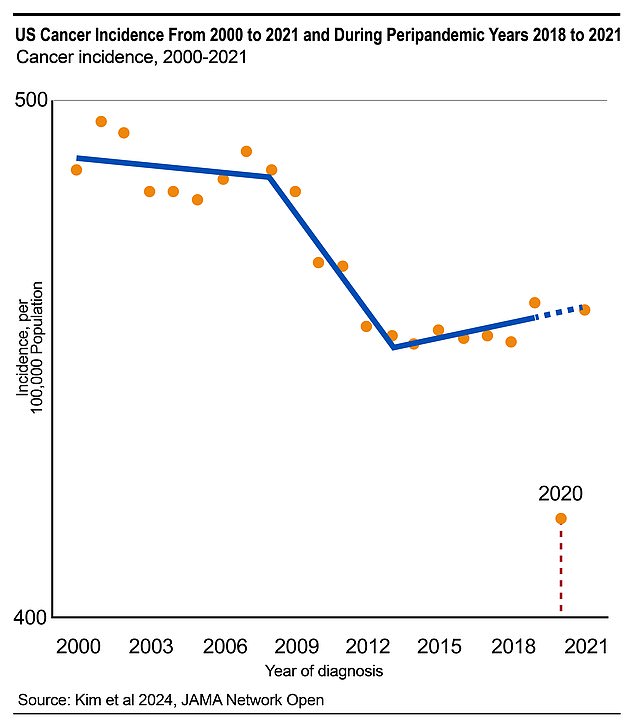
The United States is on the verge of an explosion of late-stage cancers after more than 100,000 cases were missed during the Covid pandemic.
Doctors suspected for years that health care disruptions and shutdowns led to fewer diagnoses in the early days of the pandemic.
Now, they’ve put a number on it and found that nearly 130,000 cancers were missed in 2020 and 2021, or 9 percent fewer than the expected number.
Study author Dr. Uriel Kim, a researcher at Case Western University in Ohio, said: “If cancer incidence rates do not improve further, an increase in patients with more advanced disease can be anticipated in the coming years.” .

It is recommended that breast cancer screening begin at age 45 and continue every year. Doctors recommend testing at different ages and intervals depending on sex, family history, and personal risk factors, such as smoking.
Dr. Pat Basu, The president of the American Cancer Treatment Centers, who was not involved in the study, said that from the beginning doctors focused on flattening the curve of Covid cases.
“However, another curve that is not often mentioned also requires our urgent attention: the unnoticed time bomb we call the “shadow curve” of cancer.
Researchers found that cancer diagnoses recovered to nearly meet expectations in 2021, but are still behind schedule.
During the pandemic, many screening centers closed during the lockdown, others suffered severe staff shortages.
This meant that 9.4 million screening tests that should have been performed were not performed, according to the National Cancer Institute.
This affected all medical offices. a 2021 report from The American Medical Association found that 40 percent of people admitted to missing medical appointments during the pandemic.
Even if people could go to clinics, many chose not to for fear of contracting the virus.
In the 2021 study, they found that 57 percent of respondents missed the office for fear of COVID exposure.
Collectively, doctors were preparing for the pandemic’s impact on cancer and other diseases.
They feared that missed diagnoses could create a wave of deadlier diseases, Julianne Cooleya senior statistician who studied this gap at UC Davis but who was not involved in the current research, said
Dr. Cooley said: “Because so many people with cancer did not have in-person medical care or screening, they are likely to be diagnosed at a later stage, when their prognosis is worse.”
Dr. Kim’s study, which was published in the Journal of the American Medical Association Network Open, aimed to put a number on that problem.
To do this, the team of researchers analyzed more than 15 million cases of invasive cancer between 2000 and 2021. This gave them an idea of where cancer rates would have been during the pandemic.
Their report found that 759,810 cases of cancer were diagnosed in 2020, but their modeling suggests that 127,931 cases were likely missed.
This represents a decrease of 8.6 percent for the entire year, but during some parts of the year the number of diagnoses fell by up to 50 percent.
The biggest drop occurred in lung, prostate and skin cancers. Men had a larger drop as did people in counties with low poverty rates and high education.
In 2021, rates rebounded to approach normal projections, affecting 825,645 people during the year. This was far from what doctors expected in only 2764 cases.
Dr Kim said: “Our analysis revealed that cancer detection and diagnosis improved broadly in 2021 after substantial disruptions in 2020.”
Major medical organizations, such as the American College of Surgeons and the American Cancer Society, took steps to address this concern in early 2021.

Kelsey Riddle, 32, mistook her early stage two lymphoma symptoms, which included itchy legs, for allergies.
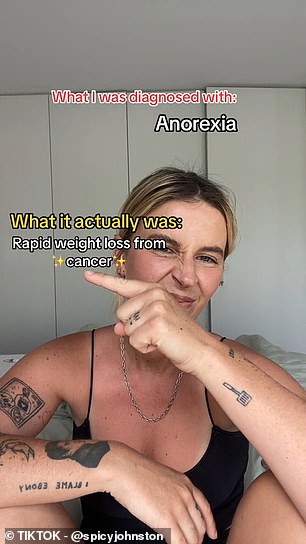
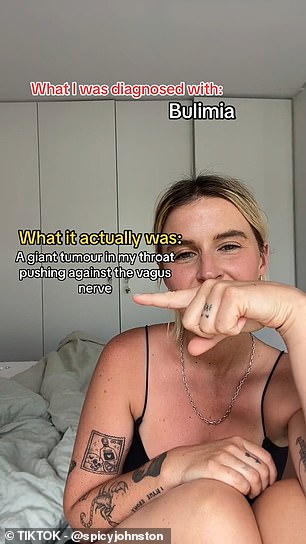
Bella Johnston, 27, was initially told by doctors that her signs of a rare throat cancer were an eating disorder like anorexia or bulimia and when she finally got the correct diagnosis, she “looked dead.”
These two paired organizations to provide support to 748 local cancer clinics to supplement their screening programs and get people back into the office.
Efforts like these could have helped flatten the curve in 2021, as could lifting the lockdown.
Cancer detection is a crucial cornerstone of modern cancer care, because detecting the disease early can mean the difference between life and death.
If cancer has the opportunity to grow in the body undetected, it can spread to more parts of the body, becoming more deep-rooted and more difficult to combat with traditional therapies.
According to the National Cancer Institute: ‘When symptoms appear, the cancer may have grown and spread. This can make the cancer more difficult to treat or cure.”
Young women, in particular, have taken to social media to share their late-stage cancer diagnoses in hopes of raising awareness about the importance of regular doctor visits and listening to your body.
Graduate student Kelsey Riddle, 32, had her stage 2 lymphoma mistaken for allergies, but she was able to beat her cancer. Bella Johnston, 27, was initially told by doctors that her signs of a rare throat cancer were an eating disorder like anorexia or bulimia, and that she “looked close to death” when she was diagnosed.
That’s why doctors recommend regular appointments to screen for diseases and other warning signs. The age and frequency of screening tests doctors recommend differ depending on age, sex, and family history.
For example, if one of your parents had early-onset colon cancer, doctors might recommend that screening begin earlier than average.
However, in general, the ACS recommends that men get screened for prostate cancer starting at age 50. Current or former smokers should start lung cancer screening at the same age.