Worsening A&E waits mean a quarter of patients seeking emergency care now face 12-hour delays at England’s busiest hospitals.
Nationwide, nearly 150,000 patients (11.3 percent) were left languishing in overcrowded emergency units for at least half a day in February alone.
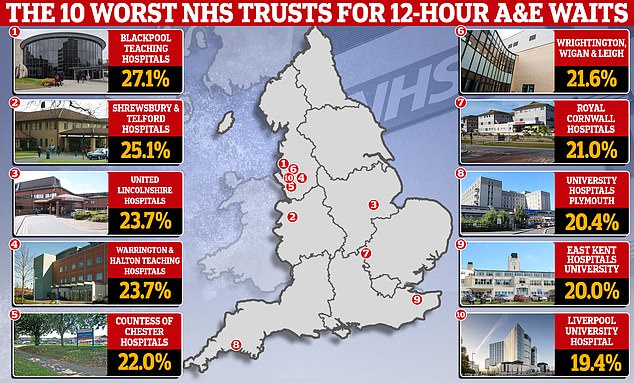
Rates were above 20 per cent in nine NHS trusts spread across Lancashire, Cornwall and Kent.
It comes after a shocking study today suggested that terrible waits in A&E for hospital beds caused more than 250 unnecessary deaths a week last year, with patients forced to wait in crowded rooms and corridors or on trolleys.
Your browser does not support iframes.
MailOnline research revealed that less than a third of patients attending A&E are seen within four hours in the country’s worst performing trusts. One in four even have to wait more than 12 hours in some NHS hospitals, illustrating the scale of the crisis, which has seen patients forced to sleep on the floor or sitting on trolleys in hospital corridors while they waited. a bed.
Dr Adrian Boyle, president of the Royal College of Emergency Medicine, said “urgent intervention” is needed to resolve the crisis.
Experts fear the situation will worsen, with the weakened NHS trapped in an “eternal winter” amid staff shortages and unprecedented demand.
Bed blocking – where patients who are fit to leave hospital cannot do so due to lack of capacity in the social care sector – and the endless schedule of strikes have only exacerbated the problem, experts say. .
NHS England figures for February show that 27.1 per cent of patients attending A&E at Blackpool Teaching Hospitals NHS Foundation Trust waited at least 12 hours from arrival to be seen.
Similarly high levels were recorded at The Shrewsbury and Telford Hospital NHS Trust (25.1 per cent), United Lincolnshire Hospitals NHS Trust and Warrington and Halton Teaching Hospitals NHS Foundation Trust (both 23.7 per cent).
For comparison, rates stood at just 0.6 per cent at Northumbria Healthcare NHS Foundation Trust.
The RCEM, using data from 5 million patients, calculated that one excess death occurred for every 72 patients who spent eight to 12 hours in the emergency room.
NHS statistics do not record the number of injured patients who spend at least eight hours waiting to be treated. However, health chiefs are recording delays of 12 hours.
Figures from last year show that more than 440,000 A&E patients in England spent 12 hours waiting for treatment.
That only counts “trolley waits”: the time between when doctors decide a patient needs to be admitted and when they actually assign them a bed.
Critics say this dramatically underplays the scale of the NHS casualty crisis, given that patients may have arrived hours before their condition was deemed serious enough for further treatment.
When this method is used, the actual number of patients who had to wait 12 hours or more in the emergency room last year is closer to 1.6 million.
About 65 per cent of waits of this length are for a hospital bed, according to an RCEM FOI.
RCEM models suggest that around 270 patients forced to wait 12 hours will have died from waiting each week. It was a slight improvement from 2022.
The figures, described as a conservative estimate, do not include the thousands of patients trapped in the back of ambulances who are also at risk of harm.
doctor boyle said: “Excessively long waits continue to put patients at risk of serious harm.”
‘Lack of hospital capacity means patients stay in A&E longer than necessary and continue to be cared for by A&E staff, often in clinically inappropriate areas such as corridors or ambulances.
‘The direct correlation between delays and mortality rates is clear. Patients are being subjected to avoidable harm.
‘Urgent intervention is needed to put people first. Patients and staff should not bear the consequences of underfunding and insufficient resources. We cannot continue to face inequalities in care, avoidable delays and deaths.’
Asked about the current figures, Dr Boyle said: “We are in a situation where being admitted to hospital will make people worse rather than better.”
Labour’s shadow home secretary Nick Thomas-Symonds said the figures were “truly shocking”.
He told GB News: ‘These are people’s lives. We have been warning about this and the dangerous situation in A&E for a long time.
‘This is not a danger that the Government has suddenly become aware of.
“This is happening, frankly, because of the lack of capacity there is now in the NHS.”
Furthermore, the latest NHS England data for February shows that no trust hospital saw all emergency department attendees within four hours.
The original goal, set in 2010, was 95 percent.
However, eight of the total 122 trusts met the weakened 76 per cent health service target.
Your browser does not support iframes.
This threshold was implemented in December 2022 and all trusts are expected to reach it by March 2024.
In a sign of the dire pressures facing the NHS, an A&E patient in Kent last year told how he was forced to endure a 45-hour wait for a ward bed to become available.
Steven Wells, a 31-year-old forklift driver, was vomiting blood when he arrived at William Harvey Hospital in Ashford, Kent, at 1am on November 13.
But they did not give him a bed in a ward until 10:00 p.m. on November 14.
Sharing a photo of him sleeping on the floor, Wells said: “Honestly, it was like a war zone at times.” It makes me not want to go back to the hospital, since the last time was very traumatic and embarrassing.
“There are people who look down on you, walk all over you, and all you want is to be taken care of.”


Steven Wells (pictured sleeping on the floor at William Harvey Hospital in Ashford, Kent) endured a 45-hour A&E wait after he began vomiting blood and was forced to sleep on the floor while waiting to be admitted.
Your browser does not support iframes.
He added: ‘They need more suitable full-time staff. There is no excuse for the way I was treated.
An NHS spokesperson said: ‘We have seen significant increases in demand for urgent services, with attendances in February up 8.6 per cent on last year and emergency admissions up 7.7 per cent.
‘The latest published data shows that our urgent and emergency care recovery plan, supported by additional funding with more beds, capacity and greater use of measures such as same-day emergency care, is delivering improvements.
‘This is in addition to ongoing work with our community and social care colleagues to discharge patients when they are medically fit to return home, freeing up beds for other patients.
“The cause of the excess deaths is due to a number of different factors, so it is only fair that ONS experts, as the executive branch of the statistical authority, continue to analyze these causes.”

