The Biden administration will dole out nearly $6 billion to states and territories to help remove toxic chemicals from the nation’s drinking water sources.
The money will fund state programs designed to remove dangerous lead pipes from the approximately 10 million homes that have them and improve wastewater treatment systems that fail to adequately clean water and make it safe to drink.
More than $1 billion will also go toward eliminating “forever chemicals” – which have been linked to cancer and fertility problems – amid growing concerns about toxins.
The administration is funneling funds from President Joe Biden’s $1 trillion infrastructure bill, passed in his first year in office.
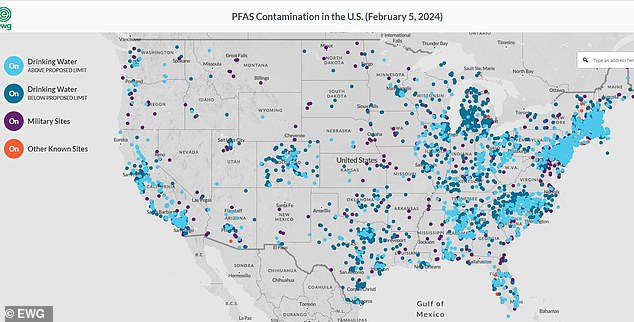
Nearly half of all tap water sources in the U.S. are laced with toxic PFAS, “forever chemicals,” which economists estimate are costing the U.S. healthcare system. between 5 billion and 63 billion dollars annually.
More than 70 million Americans drink water that has tested positive for toxic “forever chemicals,” research has shown.
The administration will give states the authority to choose exactly how water system improvement projects will be funded.
The country’s drinking water infrastructure has consistently earned below-average ratings from civil engineers, a product of decades of underfunding and the ravages of climate change.
The Biden administration is promoting the latest tranche of money as “the largest investment in drinking water in American history.”
Vice President Kamala Harris and Environmental Protection Agency Administrator Michael Regan will formally unveil the plans at an event in Pittsburgh on Tuesday.
Before the event, he said, “President Biden and I believe that everyone in our country should have the right to clean water, no matter where they live or how much money they make.”
“With this investment, we continue our urgent work to eliminate all lead pipes in the country and ensure that all Americans have access to safe, reliable drinking water.”
The federal government will not decide how the total $5.8 billion will be spent.
Instead, the money will be divided among states, which will then have the authority to choose which water improvement projects will receive funding.
EPA will oversee $3.2 billion awarded to states through the Drinking Water State Revolving Fund, which aims to improve water treatment facilities and modernize distribution networks and pipelines.
Part of that investment will include $1 billion to build seven major rural water projects to deliver new supplies of drinking water to rural communities.
Funds can also be used to replace toxic lead pipes. Although new lead pipes were banned in the 1980s, it is estimated that 12.8 million of them They still remain in buildings across the country.
Lead is a neurotoxin that, even in small amounts, can cause neurological damage and developmental delays in children.
Additionally, lead exposure can affect other systems in the body, such as the cardiovascular, kidney, and reproductive systems.
The Biden administration set a goal in 2021 to replace all of the country’s lead service lines within the decade, but cost has always been a barrier.
Still, local governments have shown that it is possible.
Pittsburgh has already received $42 million to repair its lead pipe problem through the Bipartisan Infrastructure Act of 2021. The city has successfully replaced more than 16,000 lead service lines, equivalent to more than 59 miles.

The total allocation for water system improvements as part of President Biden’s massive 2021 infrastructure bill amounts to $50 billion. The $5.8 billion announced Tuesday comes from that package.
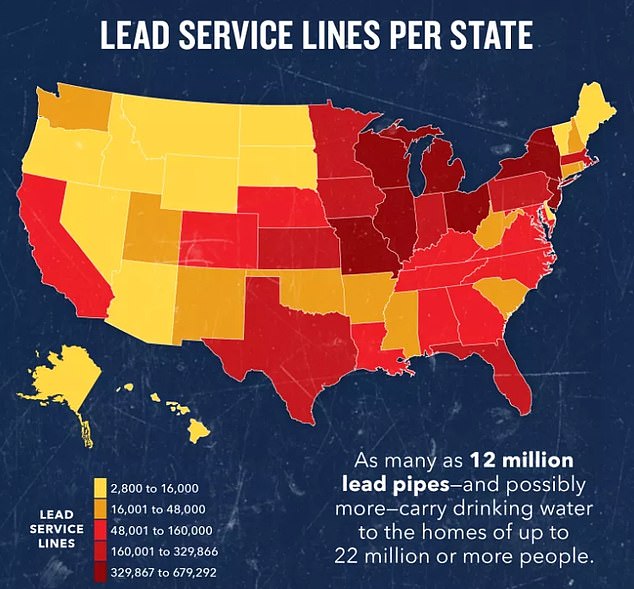
While new lead pipes are banned, there are still between nine and 13 million pipes in buildings nationwide. Map courtesy of NRDC
The latest testing showed lead levels have fallen to a record low (3.58 parts per billion), well below the state and federal threshold of 15 ppb.
The remaining $2.6 billion will be distributed to states as part of the Clean Water State Revolving Fund for a variety of projects to improve wastewater, sanitation and stormwater infrastructure. This includes $1 billion for efforts to remove PFAS chemicals and other contaminants from the water system.
The effort to remedy the PFAS problem will face difficulties. The “permanent chemicals” used in manufacturing to give raincoats, cookware, and food packaging their water- and oil-repellent qualities remain embedded in the environment for centuries before breaking down.
The White House said: “In addition, thanks to the Bipartisan Infrastructure Act, 100% of the funding to eliminate emerging contaminants like PFAS will be provided in the form of grants or forgivable loans, greatly reducing barriers for all communities with PFAS contamination.
Nearly half of all tap water sources in the U.S. are laced with PFAS. Microplastics leach into the water supply when nonstick cookware is washed, through runoff from manufacturing plants and military bases, from firefighting foam, and from landfills.