A woman has revealed how she was deceived by a man posing as Gary Barlow, who turned out to be a scammer trying to take her money.
Janet Smith, 62, from Colchester, Essex, actually believed she was speaking to the Take That singer for about a week after she added him as a friend on Facebook.
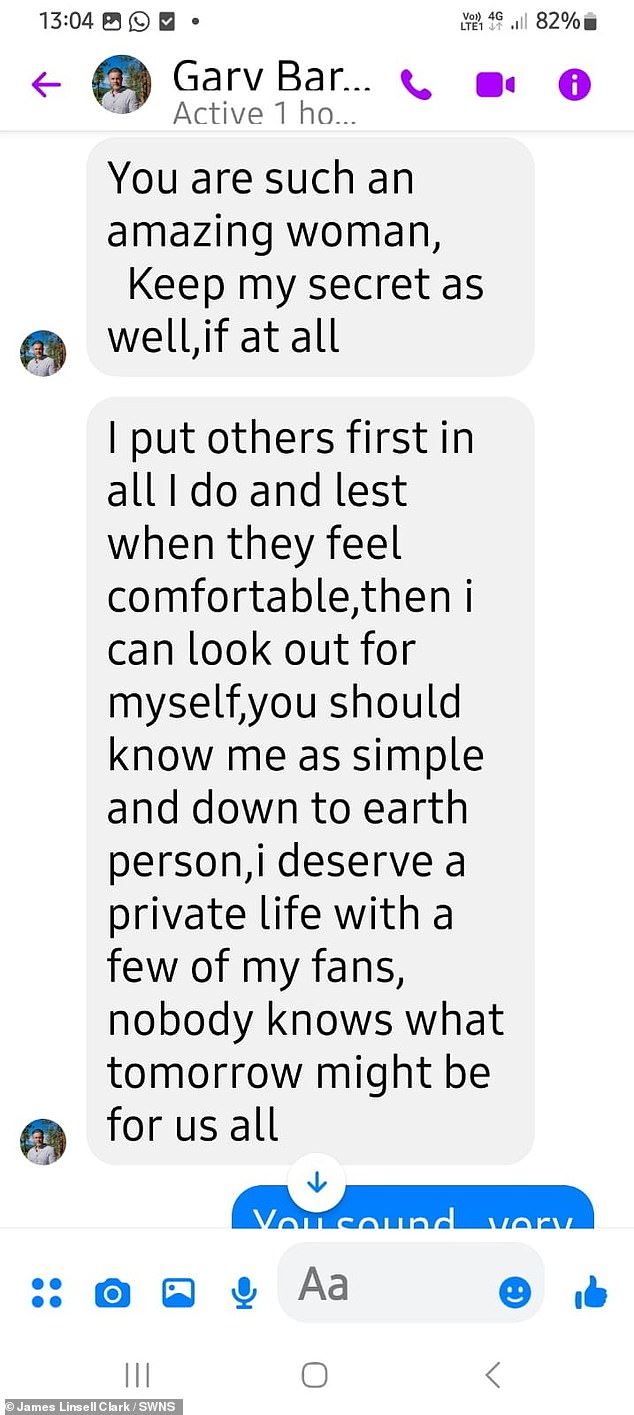
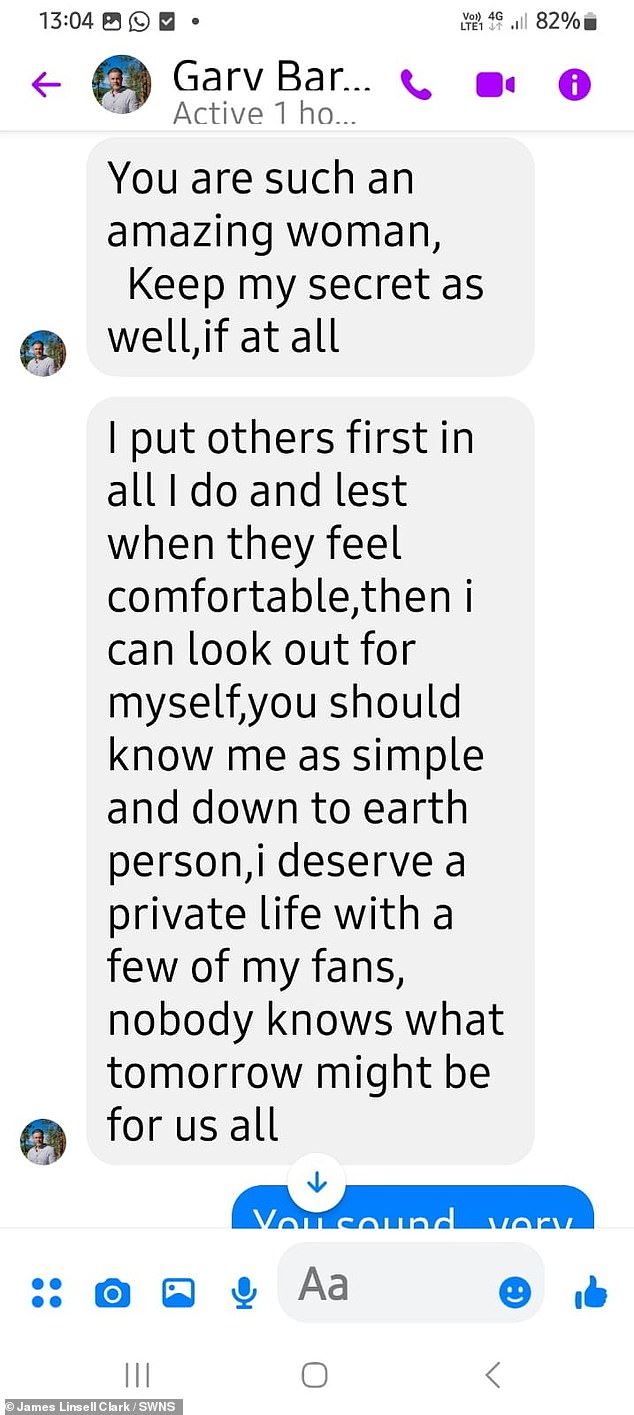
The fake Barlow bombarded her with praise and messages and said he had “separated”, which Janet took to mean his wife.
She believed she had added the pop star last month and was speaking to him all week, sometimes from 9am until 3am the next day.
In a long series of messages, he told Janet he loved her and praised her dancing in videos.
However, the scammer would interrupt the discussions by claiming to be in a meeting and rehearsing for a concert.
When he started asking for money after a few days, Janet, who works at a pizzeria, became suspicious and realized that the man she was talking to couldn’t be the real Barlow.

Janet Smith, 62, actually believed she was speaking to the Take That singer for about a week after adding him as a friend on Facebook.


Fake Gary bombarded her with praise and messages and said he had “split up,” which Janet took to mean his wife.
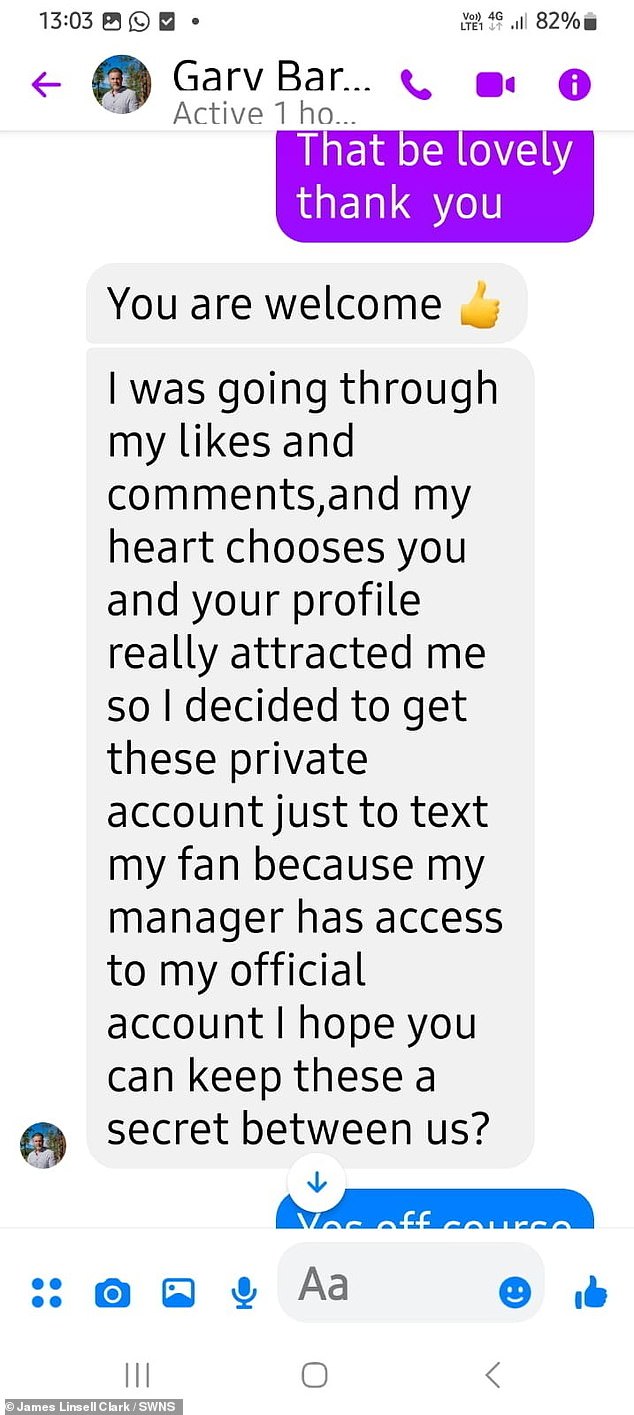
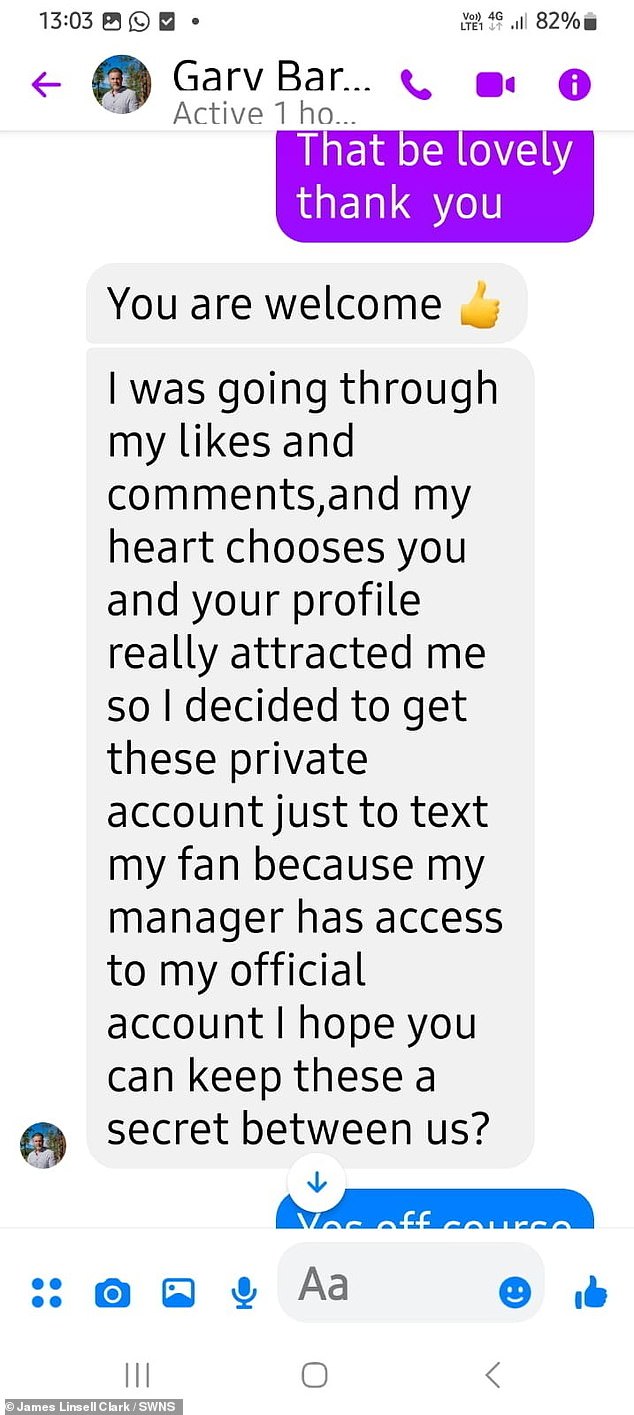
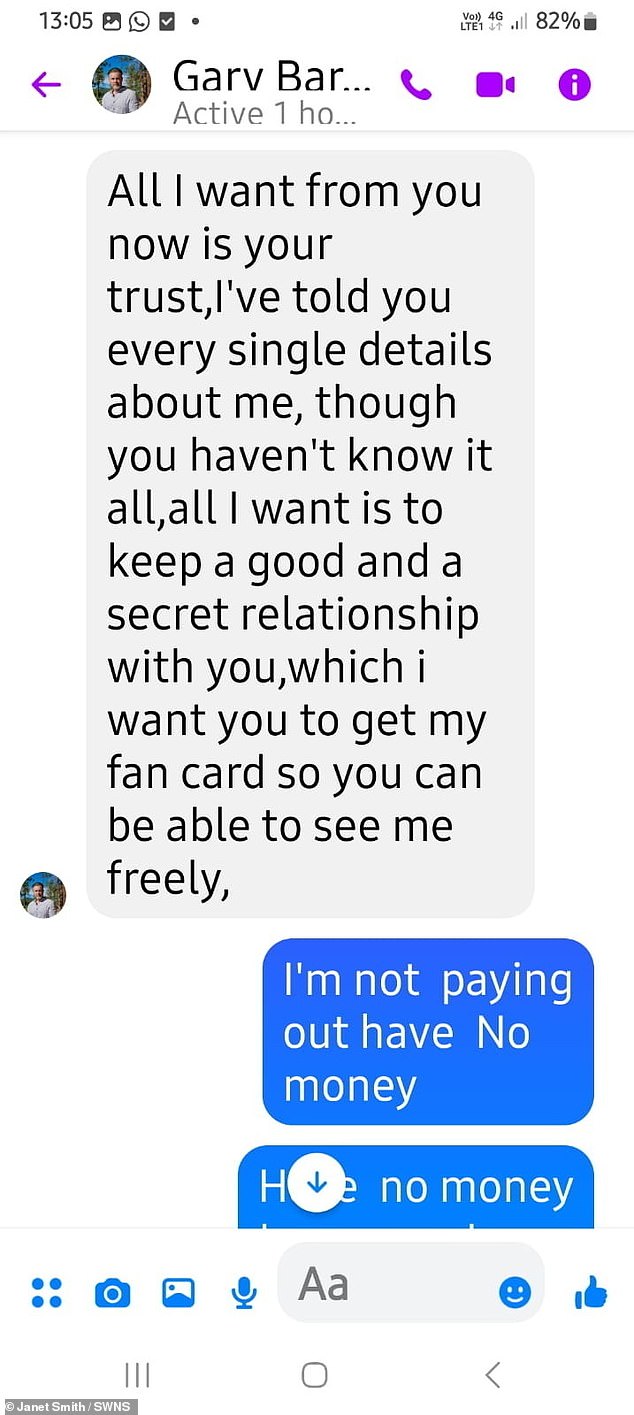
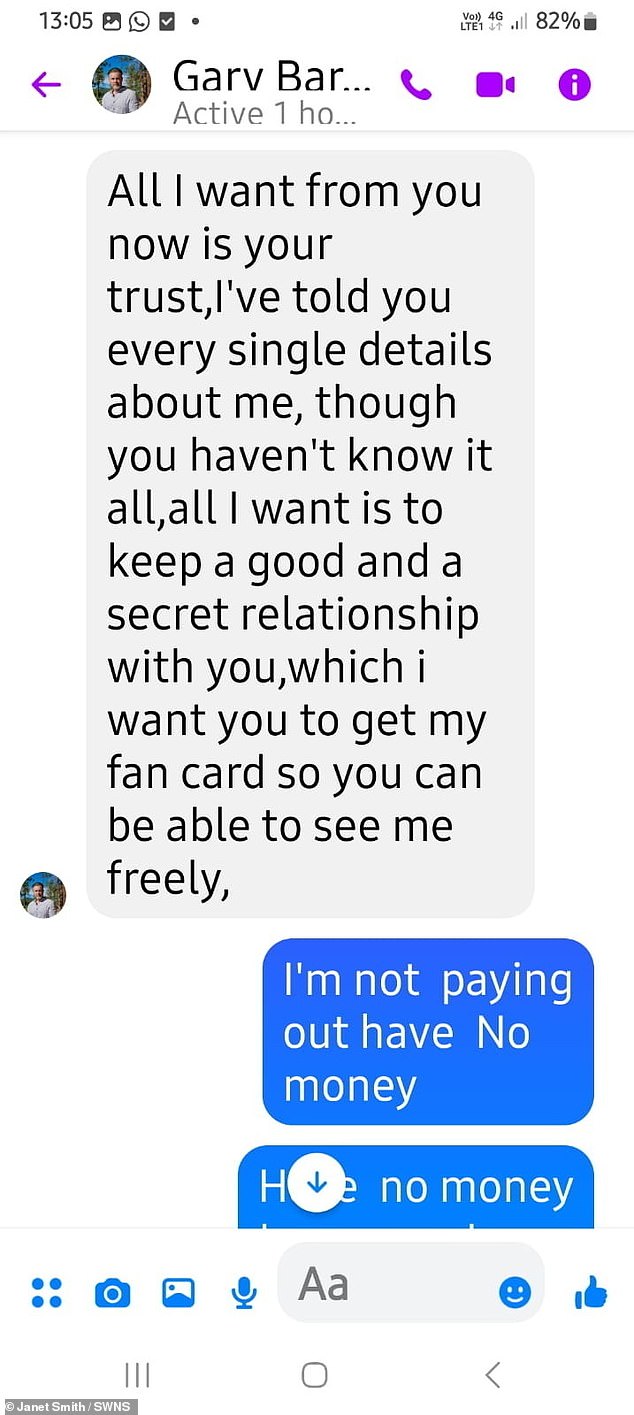
Screenshots show how the scammer told Janet ‘my heart chooses you’ and asked her to keep a secret
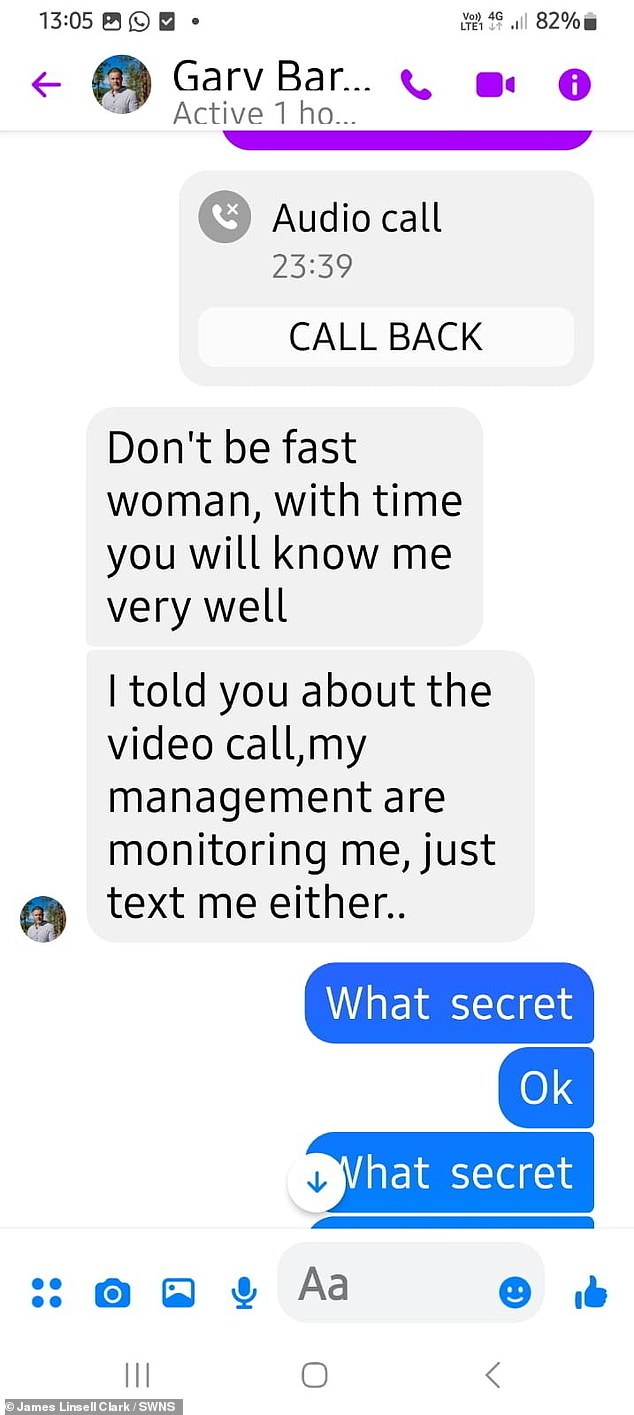
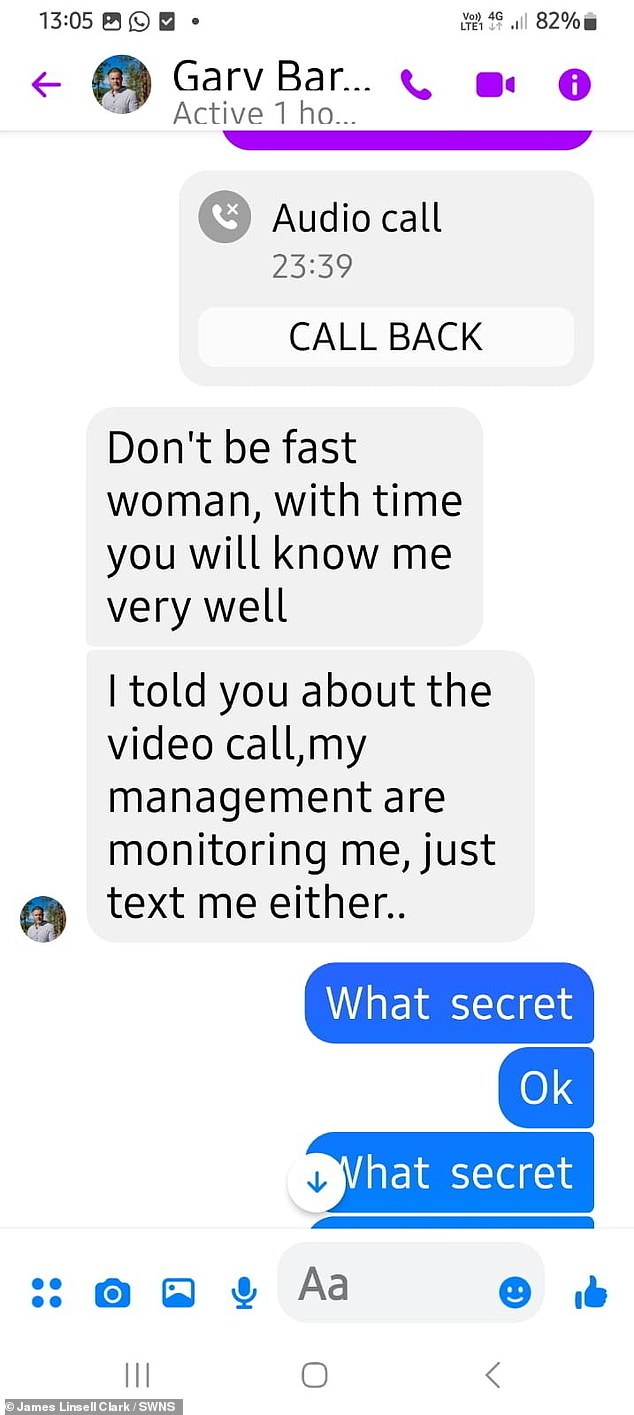
The scammer insisted Janet would “know me very well” but claimed his management was monitoring him.
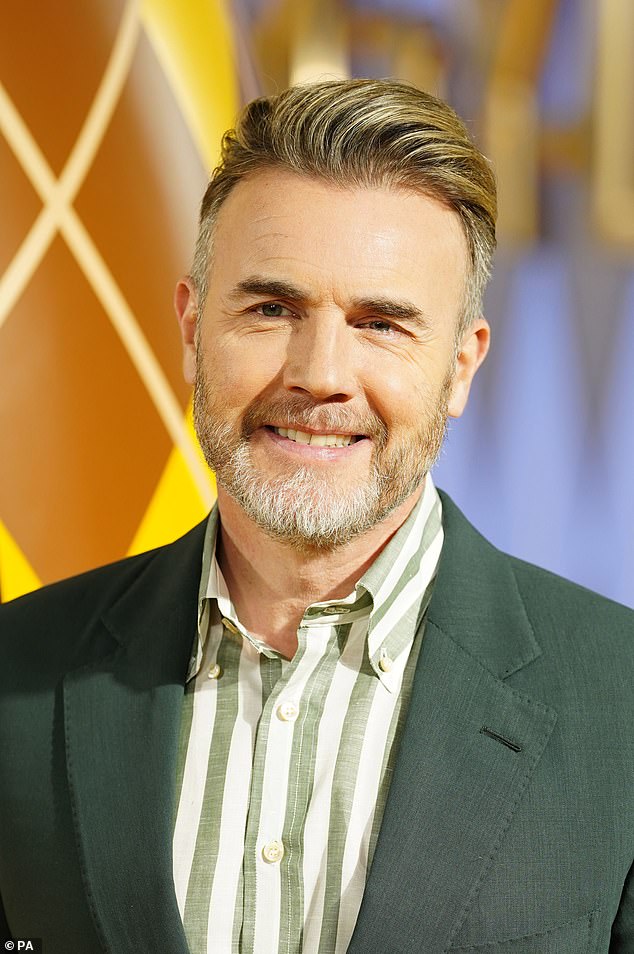
Janet initially believed she had added the real Gary Barlow (pictured in January 2024) on Facebook in March this year.
He was eventually unmasked as a 24-year-old Nigerian man.
She said: “It’s so sad because he’s been telling me ‘I love you’.”
“I said, ‘I’m 62, you’re 24.'” It makes me sad because he’s poor and he doesn’t have any money.
‘For the last week, he’s been texting me constantly, asking me where I am. She texted me from 9am to 3am’
Janet is now speaking out to raise awareness about online scammers and warn older people to be alert.
‘Older people are going to add these ‘celebrities’. They are going to scam these elderly people,” she said.
‘I understand that they are poor and have to find money for their family, but people could lose a lot of money because of this. It is also giving celebrities a bad name.”
Janet initially believed she had added the real Barlow on Facebook on March 26 this year.
“I was talking to him all week and he was like, ‘I’m busy, I have a lot of schedules,'” she said.
‘He was kind. He was good. He was really lovely and he said to me: “Good morning. Good evening, I’ve seen your videos” because I love to dance.
“The words were really fancy: ‘I’m in a meeting now’ and ‘I’m practicing for a concert.’
And everything was going well. She kept saying, “I’m Gary Barlow, I’ve broken up.”


Janet is now speaking out to raise awareness about online scammers and warn older people to be alert.
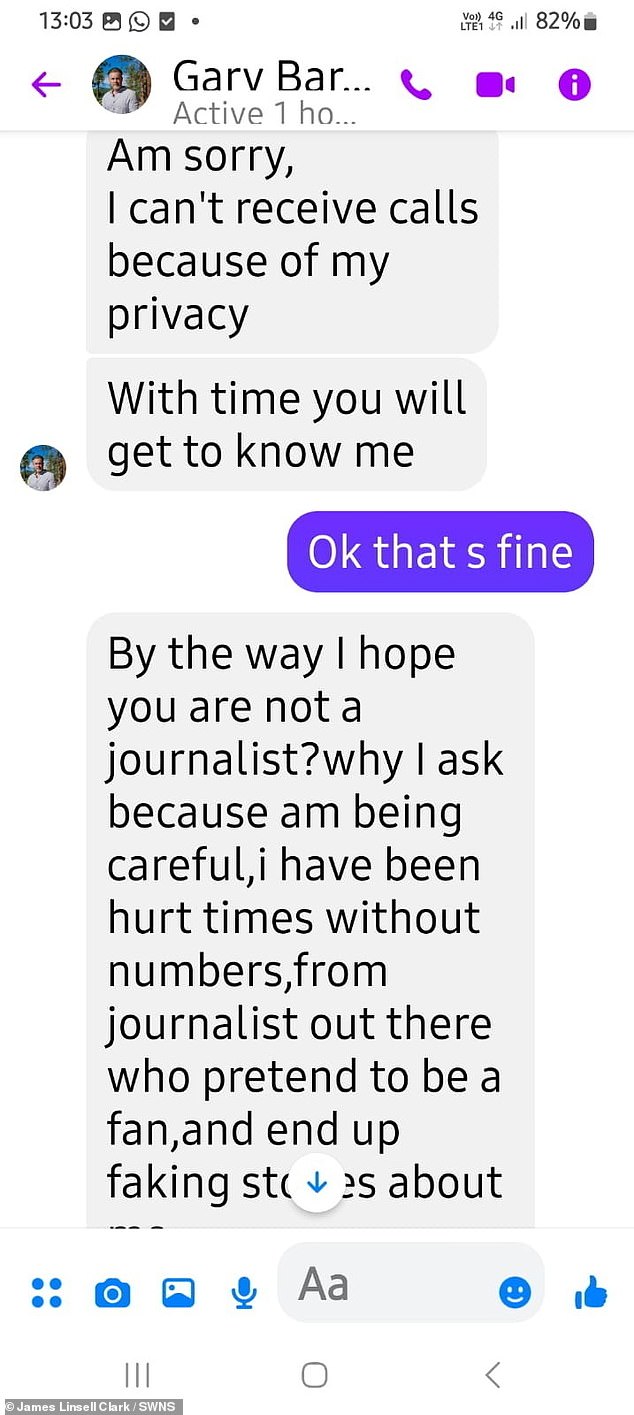
The scammer also asked if Janet was a journalist during their initial conversations.
After a few days, Janet became suspicious and realized that the man she was talking to couldn’t be the real Barlow.
“Gary Barlow wouldn’t talk to someone like me, he’s too famous,” she said. “I just thought, this isn’t Gary Barlow.”
‘I kept saying, “You’re not the real one!” And he’d say, “You’re lovely, you’re kind, yeah, I’m Gary Barlow.”
Eventually, Janet managed to persuade the scammer to reveal the truth by telling her that she could have his WhatsApp number in exchange for his true identity.
And he added: ‘He sent me a message to tell me, ‘look, I’m very sorry: I’m going to tell you the truth’ and he told me his name.
‘He is very poor. He is on WhatsApp and texts me saying, “I’m sorry I committed fraud but we come from a poor family.” I admire Gary Barlow, I like to sing and I like his songs.’
The man finally confessed his love for her.
Janet said: “He said, ‘I thought you could help me and my family, but it’s sad that you can’t.’
“I asked him what he meant by that and he said, ‘some money to get some food in Nigeria.’


Janet said she is sharing this story to help others avoid these types of scammers in the future.
After a few days, Janet became suspicious and realized that the man she was talking to couldn’t be the real Barlow.
The cheater said he was actually a 24-year-old man from Nigeria and that he was sorry for lying to the pizzeria worker in Colchester, Essex.
When Janet asked him how much he needed, his response was, “I don’t have the power to tell you how much you will give me, only you know in your heart.”
Janet told her she was “in no position to do that,” but says the whole experience made her feel “really guilty.”
Now, Janet said she is sharing this story to help others avoid these types of scammers in the future.
She said: ‘There were 20 Tom Joneses.
And Michael Barrymore has been getting closer. When they send a message, it’s similar.
“I think a lot of these foreigners do this because their countries are poor, but people think they are real celebrities.”
