Researchers in China say they have cured diabetes for the first time.
The patient, a 59-year-old man, received a pioneering cell transplant in 2021 and has been without medication since 2022.
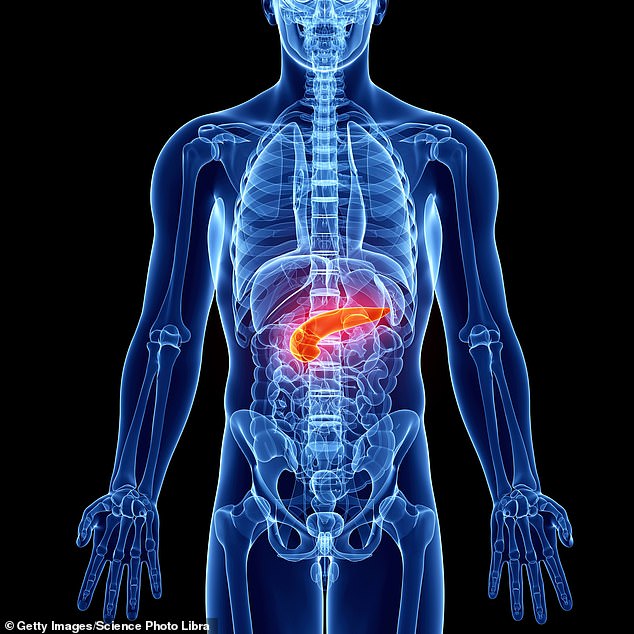
The experimental treatment involved creating an artificial version of cells found in the pancreas that produce insulin and keep blood sugar levels under control.
The man had suffered from type 2 diabetes for 25 years and had lost almost all the functions of these cells, known as islets.
He was considered at high risk for life-threatening complications and required multiple insulin injections every day to prevent him from slipping into a diabetic coma.
The pancreas is an organ that, among other functions, produces insulin. Insulin is a natural hormone that our body uses to control the amount of sugar in the bloodstream. People with diabetes have problems regulating their blood sugar level due to pancreatic dysfunction.

People with diabetes often use blood sugar monitors, like this one pictured, to determine how much sugar is currently circulating in their bloodstream. This helps them decide what to eat and when to use insulin to better control their disease.
At this point, no one has been “cured” of diabetes, but doctors have figured out how to put it into remission with diet and exercise.
But this requires patients to maintain a relatively strict diet to prevent blood sugar problems from recurring.
However, the case in China suggests that it is possible to restore the body’s ability to naturally regulate blood sugar without the patient changing their lifestyle.
The treatment used stem cells, which are a type of blank cell that can become the different types of cells the body needs to function.
Under the right conditions, stem cells can become brain, muscle, kidney, or even pancreas tissue.
This treatment used a new chemical cocktail to convert the patient’s stem cells into pancreatic cells.
These cells produce insulin, which tells the body when to extract sugar from the foods we eat for energy.
In diabetics, the pancreas does not produce enough insulin to regulate blood sugar. Too much or too little sugar in the blood can cause nerve damage, kidney damage, heart disease, and more.
By implanting new lab-grown cells, which can produce insulin, the patient could start producing their own insulin again, the researchers suggest.
This is what doctors have observed in the Chinese patient.
“I think this study represents an important advance in the field of cell therapy for diabetes,” said Timothy Kieffer, a professor of cellular and physiological sciences at the University of British Columbia in Canada, who was not involved in the research. South China Morning Post.
Although this finding is encouraging, there is still a long way to go before it can be approved for the masses.
Next, scientists will have to test their therapy in more patients.
After testing it on more people, Professor Kieffer said, they will need to find a way to scale up their operation.
Currently, converting blank “seed cells” into functional pancreatic cells is incredibly complex, time-consuming, and expensive. Scientists will have to facilitate the process if they want it to be feasible for the majority of people.
There is a possibility that it only works to treat type 2 diabetes, which is the most common form of the disease.
Type 1 diabetics, whose pancreas has been attacked by the immune system, may have more difficulty using this treatment because their immune system may reject the new implanted cells, the study authors wrote.
Regardless of all the obstacles that still remain to be overcome, this could be a big step forward for the 38.4 million Americans who currently live with diabetes and the 97.6 million who are likely to develop the disease.
It is the eighth cause of death in the country.
This article, which was published in the cell discovery magazine It is the result of decades of research, in many countries, on the best way to convert stem cells into islet cells and how to introduce those islet cells into the body.
“Our technology has matured and pushed the boundaries in the field of regenerative medicine for the treatment of diabetes,” said Dr. Yin Hao, one of the principal investigators.
The study was a collaboration between three Shanghai-based institutions: Shanghai Changzheng Hospital, the Center for Excellence in Molecular Cell Science of the Chinese Academy of Sciences, and Renji Hospital.
In the future, Professor Kieffer said this therapy could “free patients from the burden of chronic medications, improve health and quality of life, and reduce healthcare costs.”