Health authorities are sounding the alarm over the rise of six “silent killers” in the United States that are becoming resistant to the drugs normally used to treat them.
A new CDC report A study on the threats of antimicrobial resistance found that infections from six hard-to-treat germs had risen by at least 20 percent during the Covid pandemic compared with 2019 and infections remained elevated through 2022, the latest year for which data was available.
A particular problem was the rise of an antifungal-resistant fungus that can cause serious illness and is often spread in healthcare facilities. Cases of this fungus, Candida auris, increased fivefold between 2019 and 2022.
Officials estimate 29,400 people died from antimicrobial-resistant infections in 2020, but admitted that was likely a major underestimate due to underreporting, and said the 2019 count of 35,000 deaths a year was likely more accurate.
The rise is fueling concern that deaths from the once-treatable germs will rise as drugs used to fight them stop working.
Lorrie McCreary, 86, contracted Candida auris when she was transferred to a rehabilitation unit at Baycare St Anthony’s Hospital in St. Petersburg, Florida.
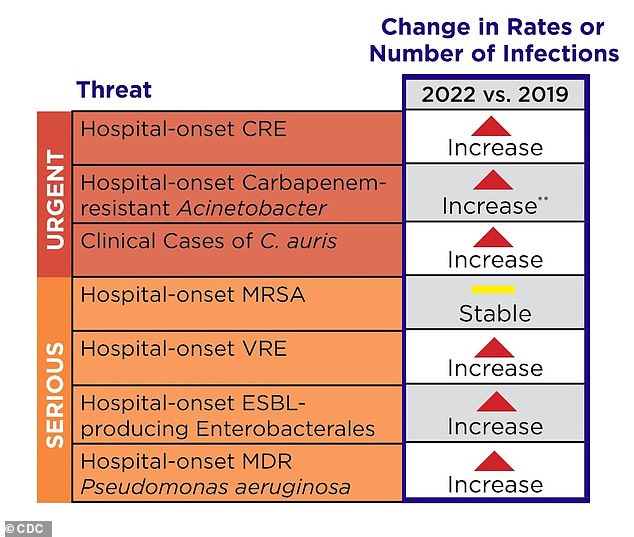
The table above shows how infections changed between 2019 and 2022 in the US.
Antimicrobial-resistant infections are those that cannot be treated with standard medications.
The CDC’s latest report looked at seven hospital pathogens and found that infections with six of them were elevated compared with years before the Covid pandemic.
Of the six, five are drug-resistant bacteria and one is a drug-resistant fungus.
These include carbapenem-resistant Enterobacteriaceae (CRE), carbapenem-resistant Acinetobacter, vancomycin-resistant Enterococcus (VRE), extended-spectrum beta-lactamases (ESBLs), multidrug-resistant Pseudomonas aeruginosa, and Candida auris (C. auris).
MRSA was the only drug-resistant pathogen of the seven whose cases remained stable between 2019 and 2022.
Poor infection control practices (such as not washing hands or changing PPE between patients) risk spreading these germs within the hospital and even beyond.
Furthermore, overuse of antibiotics increases the likelihood that pathogens will become resistant to drugs because it promotes the survival of resistant strains and facilitates their spread as other non-resistant types are eliminated.
The CDC said in its report: “The pandemic undid much of the country’s progress on antimicrobial resistance, especially in hospitals.
“The United States must continue to invest in prevention-focused public health efforts to combat antimicrobial resistance.”
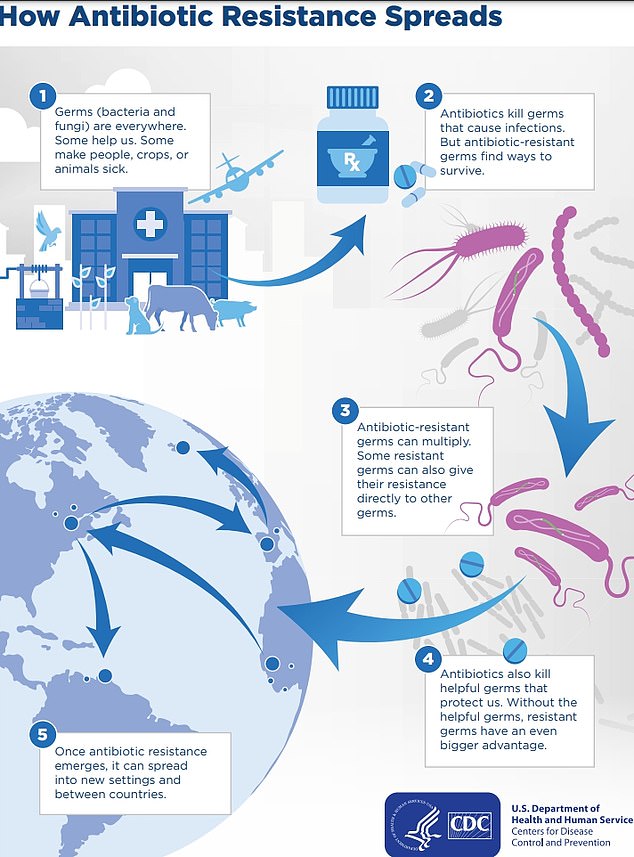
The above shows how antibiotic-resistant infections spread in the US and between countries.
Officials said Covid may have fueled the surge through longer hospital stays, shortages and increased stress on staff and resources and deteriorating infection control measures.
This would have facilitated the spread of multi-drug-resistant bacteria in hospitals, they said, increasing the risk of further infections.
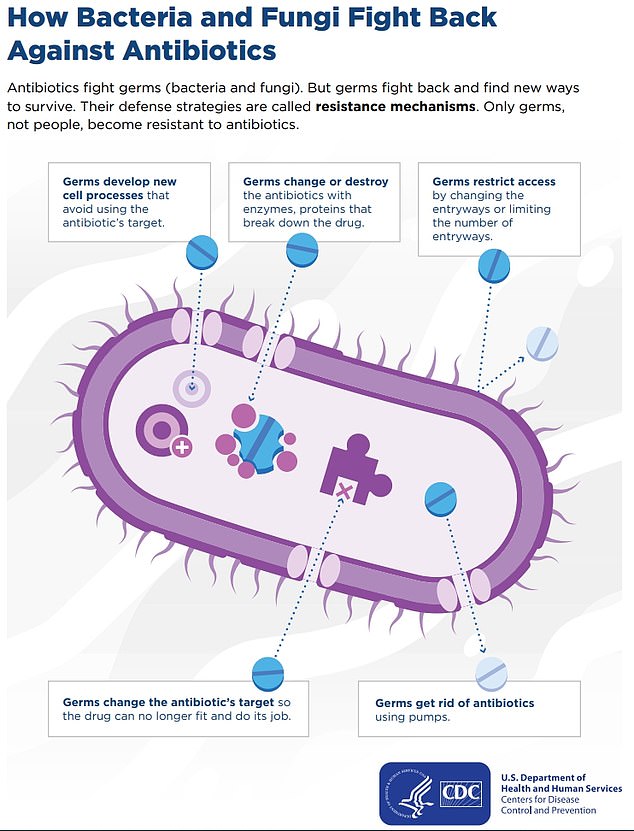
The above shows how a bacteria or fungus can fight off an antibiotic and gain immunity, rendering the drug obsolete.
Authorities were particularly concerned about the fungus C. auris, which can cause sepsis; they said cases had increased nearly fivefold over the same period.
Sepsis is a life-threatening condition that occurs when the body’s immune system overreacts to an infection, triggering severe inflammation that causes organs to shut down.
Up to a third of patients with this disease do not survive.
Among the patients who contracted C. auris as a result of the pandemic was Lorrie McCreary, who died from the infection in June 2022.
The 86-year-old man was originally admitted to hospital with pneumonia and appeared to be recovering well.
But his condition deteriorated rapidly, forcing his doctor to run a series of tests that revealed the fungus, which he is believed to have contracted while in hospital, likely through an oxygen tube.
A fatal chain of events was set off, leading to sepsis, kidney failure and a fatal stroke.
Her daughter Sharon, 61, said she felt her mother would still be alive if she had not contracted the infection.
In the case of MRSA, there are more than 80,000 cases and 11,000 deaths each year in the United States, the data show.
For the report, CDC analyzed data on seven antimicrobial-resistant infections submitted by hospitals and laboratories across the country.
The report also found that during the Covid pandemic, nearly 80 percent of hospitalized Covid patients received an antibiotic between March and October 2020.
This was initially due to difficulties in distinguishing Covid from community-acquired pneumonia in the early days, officials said.
But antibiotics will not work against Covid because they are designed to attack bacteria and not the virus.


