Aging baby boomers are finding that their carefree youth is catching up with them as alcohol consumption takes its toll on the “substance abuse generation.”
There was a 237 percent increase in alcohol-related deaths among people over 55 between 1999 and 2020, and the stress of the pandemic has made things worse.
The crisis makes no distinction by social status and the wealthy are at least as vulnerable, and analysts have warned that the country faces a public health crisis as boomers flood emergency rooms.
“If Baby Boomers consumed alcohol at the same levels as the previous generation, their group size would lead to a significant increase in alcohol-related harms,” wrote Dr. George Koob of the National Institute on Alcohol Abuse and Alcoholism. .
“While the prevalence of alcohol consumption in this age group increased by only 15.7 percent, the actual number of drinkers increased by 80.2 percent.”

There was a 237 percent increase in alcohol-related deaths among people over 55 between 1999 and 2020, and the stress of the pandemic has made things worse (file image)
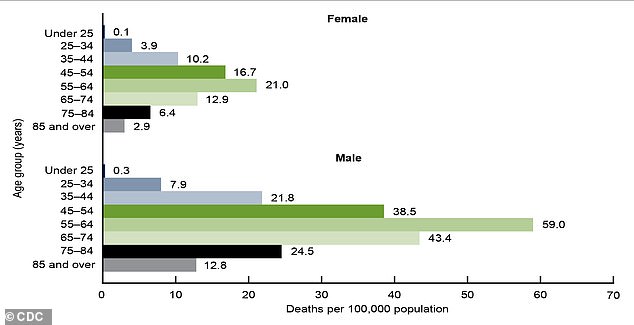
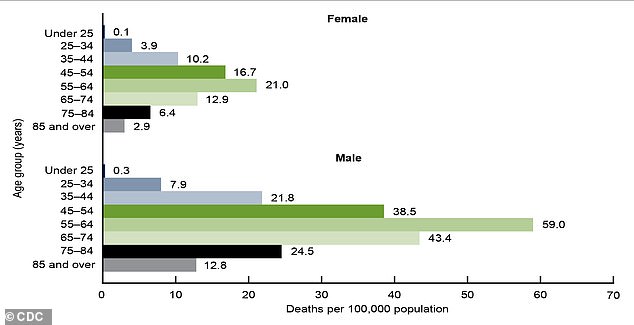
Alcohol-related deaths among boomers easily surpassed those of other age groups among men and women in 2020, according to CDC data.
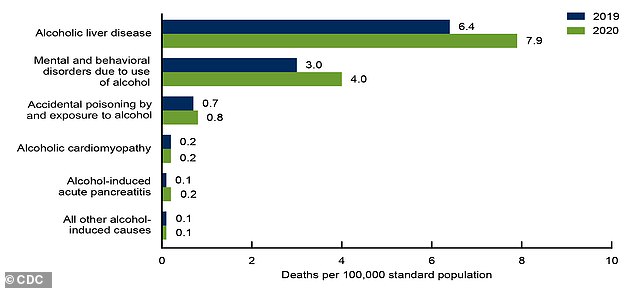
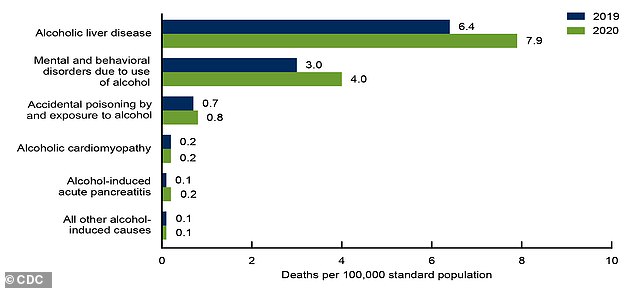
Liver damage remains by far the most lethal effect of alcohol among long-term users
Alcohol consumption peaked in the United States in 1980, when boomers were in their prime.
But rather than reducing consumption, older Americans appear to be doubling down on the bad habits of their youth, with binge drinking in that age group increasing 40 percent in the 15 years to 2018.
And women are rapidly closing the gap with men when it comes to both alcohol consumption and binge drinking.
The amount of alcohol drunk by older men grew by 0.7 percent annually between 1997 and 2014, but by 1.6 percent annually among women.
“Boomers are a substance-using generation,” Keith Humphreys, a psychologist and addictions researcher at Stanford, told the conference. New York Times.
“Women have been the drivers of change in this age group.”
She said boomer women entered the workplace in large numbers at a time when drinking was central to the culture and people had more disposable income.
“Contrary to stereotypes, educated and upper-middle class people have higher rates of alcohol consumption,” he explained.
“Women retiring now are more likely to drink than their mothers and grandmothers.”
A survey conducted in May 2020 found that one in 10 older adults were drinking more each week than before, and that the odds of increased drinking were twice as high if a respondent reported loneliness or had symptoms of anxiety or depression (file image)
More than 178,000 Americans died from alcohol in 2021, an increase of nearly a third in just two years.
38 per cent of them were over 65, but experts fear the true cost of the pandemic has yet to emerge as the impact of alcohol consumption during lockdown is felt.
Deaths directly attributable to alcohol, emergency room visits, and per capita alcohol sales skyrocketed as COVID restrictions were imposed.
A survey conducted in May 2020 found that one in 10 older adults were drinking more each week than before, and that the odds of increased drinking were twice as high if a respondent reported loneliness or had symptoms of anxiety or depression.
And if someone had all three (loneliness, anxiety and depression), they were 3.8 times more likely to drink more.
“We were hit by a lot of stressors: the isolation, the worry about getting sick,” Dr. Koob said.
“They point out that people drink more to cope with that stress.”
And experts fear that aging boomers are unaware that their bodies can no longer handle alcohol as well as they once did.
“Equivalent amounts of alcohol have much more disastrous consequences for older adults,” said Dr. David Oslin of the Philadelphia Veterans Affairs Medical Center.
“It causes slower thinking, slower reaction time and lower cognitive ability when you’re older, it exacerbates cardiovascular disease, kidney disease and, if you’ve been drinking for many years, there’s an increase in certain types of cancers.” .
And he worries that older people are becoming complacent about drinking alcohol while under the influence of the medications they increasingly have to take to deal with age-related conditions.
Pain relievers and sleeping pills can cause excessive sedation if mixed with alcohol, and waiting a few hours before having a drink may not be enough.
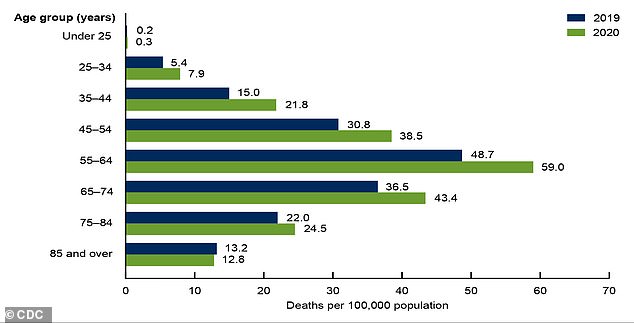
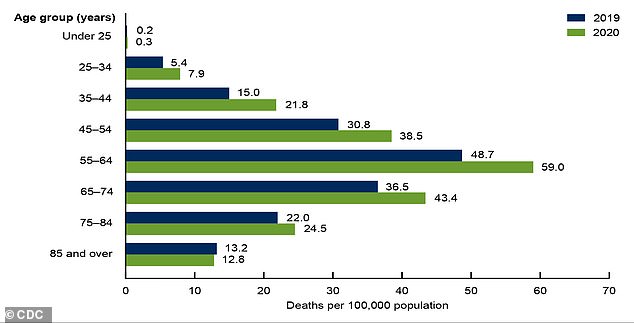
Alcohol-related deaths have increased during the pandemic among men ages 55 to 64, according to the latest data from the National Center for Health Statistics, and are expected to rise further as the impact of restrictions unfolds.
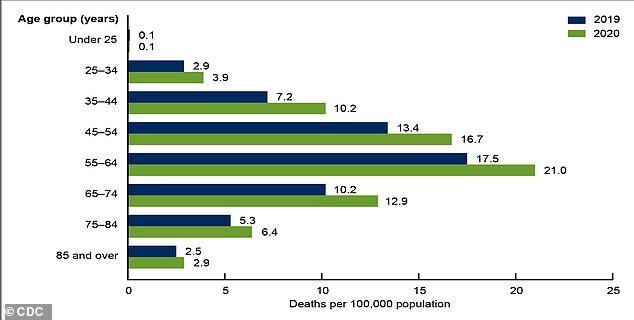
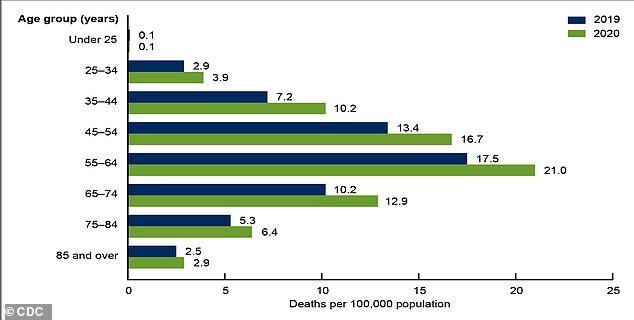
The figures are no less alarming for women who are beginning to catch up with men
“Those medications are in your system all day long, so when you drink, there’s still that interaction,” he added.
But it’s difficult for many to access help because the Medicare that many seniors rely on doesn’t offer the same coverage for substance use disorders as it does for other medical conditions.
“In fact, age is the best predictor of a positive response,” Dr. Oslin said.
‘Treatment does not necessarily mean that one has to become abstinent. We work with people to moderate their alcohol consumption.’
