A “greedy and grotesque” Los Angeles woman who was caught in an elaborate squatting scheme has been sentenced to 20 years in prison.
Carolina Herrling, also known as Carrie Phenix, 44, of West Hills, was sentenced Friday by a U.S. district judge for targeting elderly men and taking over their million-dollar mansions.
Herrling was also accused of disposing of a victim’s body after she died in a home she quickly called her own.
In 2020, she found a palatial home in Sherman Oaks owned by 71-year-old Charles Wilding, broke in, discovered his dead body, took over the house and disposed of his remains.
The following year, Herrling decided to fraudulently sell a mansion in Encino that belonged to 53-year-old Robert Tascon. He committed suicide on September 11, 2022.
“This lady is a great manipulator and con artist and she managed to use the dead.” Hold her accountable and don’t let her do this to anyone else,” Tascon’s heartbroken partner Miracle Williams told the Los Angeles Times.

Carolina Herrling, also known as Carrie Phenix, 44, of West Hills, was sentenced Friday by a U.S. district judge for targeting elderly men and taking over their million-dollar mansions.
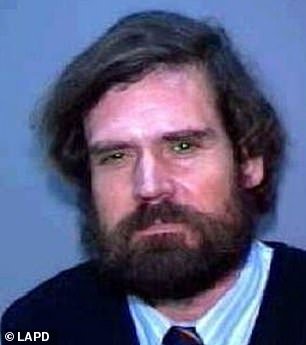
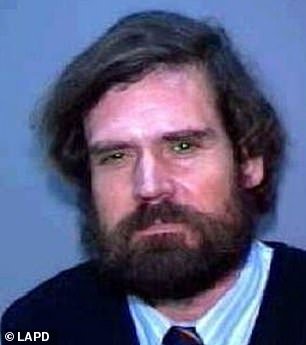


In 2020, she found a palatial home in Sherman Oaks owned by Charles Wilding (left), broke in, discovered his corpse, and took over the house while it rotted. In 2021, she fraudulently sold a mansion in Encino that belonged to Robert Tascon (right)
According to the U.S. Department of Justice, Herrling pleaded guilty last year to a federal charge of conspiracy to commit wire fraud.
She was also ordered to pay $3.88 million in restitution costs for her crimes.
“This defendant’s misconduct was both greedy and grotesque, causing deep pain to the victims and their loved ones,” U.S. Attorney Martin Estrada said in a press release.
“There must be serious consequences for those who prey on vulnerable communities, such as the elderly, and my office will remain committed to bringing these offenders to justice.” »
Court documents revealed that Herrling and his co-conspirators “preyed on vulnerable victims” who lived in wealthy neighborhoods and resided in homes that “appeared poorly maintained.”
To do this, she and her team would use online mapping programs and visit wealthy neighborhoods looking for properties with overgrown shrubs and algae-filled swimming pools to identify victims, the press release said.
In 2020, when she stumbled upon Wilding’s home in Sherman Oaks Mansion, she and her associates broke into the house before calling it their own.
“Sometime in September 2020, the victim died – investigators are unsure how – and they believe Herrling and others took over the property while her body decomposed in her home,” the statement said Press.
Instead of reporting her corpse, Herrling and his team stole all of her belongings while her body rotted inside the house.
According to the release, Herrling used a “fake power of attorney form” and pretended to work on Wilding’s behalf while she stole from his home and took over his financial accounts.


When Tascon briefly left his home to live with his partner after developing a drinking problem, Herrling moved into his mansion and sold it. (Photo: The former Tascon Mansion located at 5309 Louise Ave in Encino, CA)
In 2021, the victim’s neighbors reported Wilding missing and police began investigating.
Once they got their hands on Herrling, she told them she was a “close friend” of hers who had been listed as a trustee of her family trust which had been forged to resemble her mother, who died in 2017 , created court documents. said.
She later told authorities that Wilding had moved from Sherman Oaks to Carpinteria, even though she thought he was already dead.
Investigators quickly discovered that Herrling and his co-conspirators had moved the victim’s body to his West Los Angeles apartment and attempted to dissolve it with chemicals.
When that plan failed, the scheming team decided to dismember Wilding’s body throughout the Bay Area. One member of his crew even took his sailboat into San Francisco Bay and dropped parts of his body into the water.
Wilding’s remains were never found, the news release said.


After his death, police discovered that Tascono had a history of mental illness and was involved in fraud litigation (photo: Tascon seen in undated photo)
During Herrling’s hearing, Judge Maame Ewusi-Mensah Frimpong said Wilding was “a man and a human being” and that Herrling treated him more “like a cash register.”
Prosecutors said Wilding was listed as another victim’s beneficiary and executor, but that the document Herrling claimed to have “discovered” in a safe rented by his deceased mother was also forged by her.
Court documents revealed that, according to the fake will, the missing victim was to inherit an estate worth more than $1.7 million, assets that fell under Herrling’s control as “fiduciary” of the inheritance.
In 2022, she and her associates defrauded Tascon, a man from a wealthy family who had set up two trusts for him, according to a United States Postal Inspection Service report.
He briefly left his home to live with his partner after developing a drinking problem, Travis Hargraves, Tascon’s attorney and case manager, told the Los Angeles Times.
Meanwhile, Herrling moved into her mansion and with fake documents and another fake will, she posed as Tascon, created accounts, sold her house for $1.5 million and pocketed the money from the sale.
According to the affidavit, she used that money to buy a house in West Hills.


Herrling pleaded guilty last year to a federal charge of conspiracy to commit wire fraud. She was also ordered to pay $3.88 million in restitution costs for her crimes.


Court documents revealed that Herrling and his co-conspirators “preyed on vulnerable victims” who lived in wealthy neighborhoods and resided in homes that “appeared poorly maintained.”
According to Hargraves, the house was one of his client’s remaining assets, along with monthly payments from his trusts.
After the sale was completed, Tascon became embroiled in a vicious legal battle with Herrling and filed a lawsuit against her.
Hartgraves remembers his client telling him he feared he would never get his house back.
“The fraudulent sale almost crushed him,” Hartgraves told Lyndon Versoza, a postal investigator involved in the case.
The victim committed suicide in September and, according to the police report, he had a history of metal disease and was involved in fraud litigation.
Herrling said she was not involved in the sale of Tascon’s house and was only paid $150 to facilitate the sale through the notary.
She was unable to describe Tascon and claimed she didn’t take everything from him, the affidavit states.
Assistant U.S. Attorney Andrew Brown said Tascon “owned property and he lost it.”
In October 2023, one of Herrling’s accomplices, Matthew Jason Kroth, 50, pleaded guilty to one count of conspiracy to commit wire fraud and one count of possession with intent to distribute methamphetamine.
Kroth faces up to two decades in federal prison for the wire fraud charge and up to 40 years for his meth charge.