A woman diagnosed with ovarian cancer has claimed she was “gaslit” by doctors after they dismissed her pelvic pain as simply “part of being a woman”.
Keesha Walden, from Norfolk, began experiencing sharp pains on her left side in early 2023, at age 26.
But in March she began experiencing excruciating pains in her lower abdomen and irregular periods. However, she said her GP had told her she simply needed to watch her diet and exercise.
It was only after her symptoms worsened that she was sent to gynaecology as an urgent cancer referral in September, where they found what they believed to be a cyst on her ovary.
Surgery to remove it a month later showed he had a cancerous tumour measuring 26cm – about the size of a rugby ball.
Keesha Walden suffered from severe pelvic pain that was a hidden sign of a large ovarian cancer.
Follow-up scans in February showed the cancer had spread, with a new mass in the pelvis and abnormal tissue in the lung.
She was diagnosed with mucinous adenocarcinoma, so rare that it accounts for only three percent of all ovarian cancer cases.
Recalling her harrowing experience, she said: “Due to the late diagnosis, I was informed that a hysterectomy was my only option for survival and that they suspected the cancer was in fact stage three, potentially stage four.”
‘I was told that all my checks were fine and everything was healthy, even though the GP never saw me face to face, and told me to be careful about what I ate and exercised as my BMI was perfect but my waist circumference was very large.’
‘One of the most damaging ways doctors misled me was when they repeatedly dismissed my symptoms, despite me telling them how severe my pain and discomfort was.
“This made me doubt my own experience and delayed the proper diagnosis and treatment I needed.”

The 27-year-old sales consultant revealed her massive abdominal bloat, another telltale sign of the ovarian tumor hidden in her pelvis.
She added: ‘I was told I was ‘too young’ to have a serious condition, especially when it came to something like ovarian cancer.
‘I was ignored and assured that my symptoms were probably nothing to worry about due to my age. This assumption led to a significant delay.
There were times when doctors suggested my symptoms were due to poor lifestyle choices, without considering other possibilities.
‘They suggested that I simply needed to eat better, exercise more or relax, which made me feel responsible for my own suffering and prevented them from looking more deeply at the real cause.
‘One of the most disheartening cases of psychological manipulation I experienced was when I asked my doctor about the five-year survival rate.
‘She responded condescendingly, saying, “They’re just numbers,” as if my concerns were irrelevant or silly.
‘When I pressed for more information, she vaguely assured me that she was ‘pretty sure’ I would be discharged in five years, but offered no further clarity.
‘His inability to give a concrete answer, combined with his dismissive attitude, made me feel foolish for even asking.
He concluded by saying: “Sometimes doctors don’t have all the answers.”
“That made me feel even more anxious, as it seemed like she was downplaying the severity of my concerns.”
Ovarian cancer is the sixth most common cancer in the UK.

Ms. Walden had to undergo a major procedure to remove the cancer, which included removing several of her pelvic organs.
The disease kills about 11 women every day in Britain, on average, or 4,000 a year.
It also kills three times as many women in the United States each year, figures show.
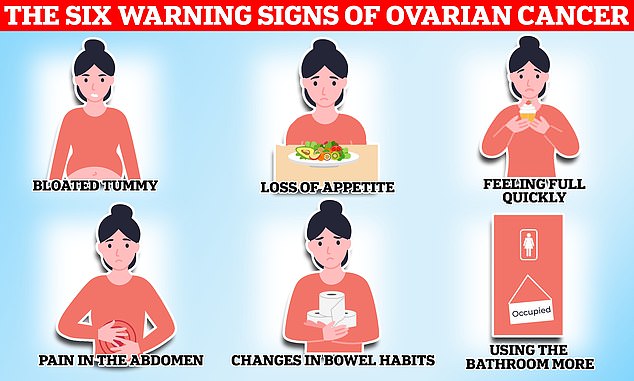
It is often diagnosed late because symptoms are vague and may include indigestion, pelvic or abdominal pain, loss of appetite, constipation, and increased need to urinate.
About 93 percent of women diagnosed live five years or more if detected at the earliest stage, compared with just 13 percent diagnosed at stage four.
Stage three means that the cancer has spread outside the pelvis to the abdominal cavity or to the lymph nodes.
About one-fifth of women with ovarian cancer are also diagnosed in emergency rooms, often when it is too late for any treatment.
In March, Ms. Walden underwent a total abdominal hysterectomy, in which both ovaries, both tubes, uterus, appendix, cervix, 26 lymph nodes and omentum were removed.
She said: ‘I’m currently still on chemotherapy, hoping for my last cycle on September 6.

She was diagnosed with mucinous adenocarcinoma, so rare that it accounts for only three percent of all ovarian cancer cases.

Ms Walden said: “Cancer and chemotherapy have deeply affected my confidence and self-esteem as a woman. The physical changes that come with treatment, hair loss, weight fluctuations and visible wear and tear on my body and extensive scarring have been difficult to come to terms with.”
‘After that, I’ll have to face a five-year follow-up period to see if the nodules in my lung change and to ensure there are no other signs of recurrent disease.
‘The uncertainty of my situation makes it difficult to imagine what my future will be like.
‘At 27, most people are focused on building their lives, buying a house, settling down and starting a family.
“Unfortunately, all of that has been taken away from me. My new reality is finding peace with the unknown.”
She added: “Cancer and chemotherapy have deeply impacted my confidence and self-esteem as a woman.
‘The physical changes that come with treatment, hair loss, weight fluctuations and the visible impact on my body and large scars have been difficult to accept.
‘These changes have often left me feeling disconnected from the person I once was, struggling to recognise myself in the mirror.’
According to the NHS, staff shortages and workload were the reasons attributed to the late diagnosis.
“There is a great deal of misunderstanding about current reporting processes and the role of the cancer center,” they added.
“There is no effective safety mechanism in gynecology to detect abnormal results. This is a problem that affects everyone.”
Ms Walden said: “This experience has changed me irrevocably. While I hope to find peace, the uncertainty of whether I even have five years left to live adds to the emotional turmoil.

Now Ms. Walden is urging others to demand answers from their doctors and not to give up on seeking a diagnosis.
Ovarian cancer is a rare form of the disease that develops in the ovaries, the female organs that produce eggs. It is often called the “silent killer” because symptoms do not appear until the later stages of the disease.
“Everyone couldn’t believe that this could happen to me at such a young age”
‘There was anger that it hadn’t been detected sooner, especially after having struggled with my health for so long and being given false assurances throughout the process.
‘It was a crazy and overwhelming time for me and my family. The delay in results meant that everything suddenly became urgent; there was no time to pause and process what was happening.
“It was a surreal and terrifying experience for all of us.”
Now Ms. Walden is urging others to demand answers from their doctors and not to give up on getting a diagnosis.
‘Now I still have nodules in my lung that have not been analyzed, the hospital has no plans to perform a biopsy because they are apparently too small (five millimeters) and they cannot yet confirm whether they are cancerous or not.
‘But my trust in the NHS is non-existent now, given the misdiagnosis and delay in the application of results.
“To everyone facing the challenges of cancer and chemotherapy, I know this journey can feel overwhelming, but remember that you are stronger than you think,” Keesha said.
‘Every day you fight is a testament to your resilience and courage.
‘Your worth is not defined by the changes in your body or the struggles you face, but by the incredible strength you demonstrate in the face of them.
“Always listen to your body, if you feel like something is not right, make sure to push and follow up. I regret not being more persistent in getting a diagnosis.”

