The death of a Michigan chef from a fungal infection has shed light on a silent epidemic that has been growing in the United States for years.
In particular, four deadly strains have become more common in recent decades. infecting thousands of people now compared to just dozens in the early 2000s.
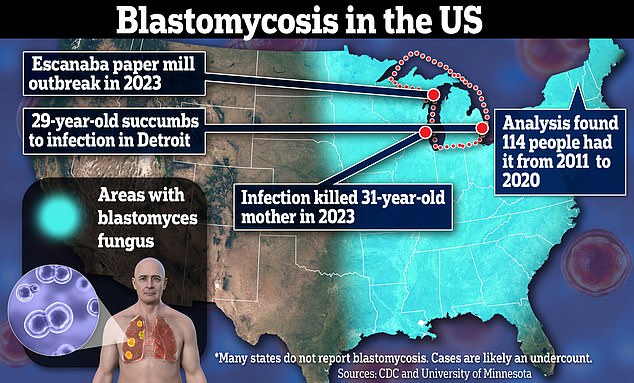
DailyMail.com revealed the latest victim of the outbreak earlier this week, Ian Pritchard, 29, whose lungs were “devastated” by blastomycosis, a microscopic yeast that spreads when people inhale its spores.
The fungus hides in moist soils and rotting wood in the upper Midwest, but global warming has allowed it to flourish on the East Coast as well.
Meanwhile, in the West, Valley fever is making more people sick than ever, with cases in California tripling from 2014 to 2018 and from 2018 to 2022.
Since reporting on Ian Pritchard’s death, DailyMail.com has heard from other people whose loved ones or themselves have fallen victim to life-threatening fungal infections.
Blastomycosis usually arises from exposure to humid environments, primarily in the upper Midwest. But epidemiological studies are increasingly finding the fungus on the East Coast.
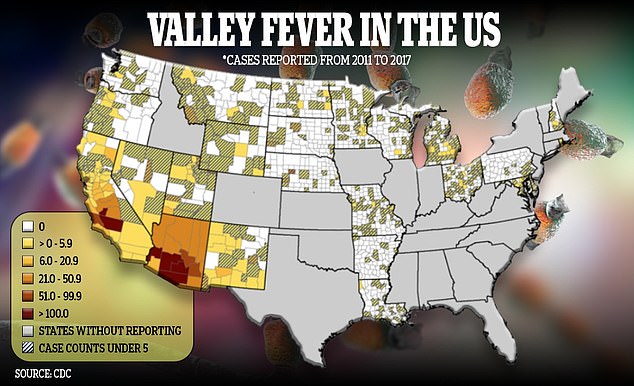
The fungus that causes Valley fever thrives in hot, dry environments

Ian Pritchard was in a medically induced coma in a Detroit hospital before passing away over the weekend. Doctors were unable to eradicate the fungal infection, which would have prepared Ian for a life-saving lung transplant.
The Centers for Disease Control and Prevention, as well as the World Health Organization, have raised alarm bells in recent years about pathogenic fungi that can evade medications.
Climate change, along with international travel, makes the spread of potentially dangerous pathogens, including fungal strains, more likely.
An estimate 7,199 deaths from fungal diseases occurred in 2021, according to the CDC. That’s up from a total of 5,922 deaths the year before and 4,833 deaths the year before.
Ian Pritchard’s case of blastomycosis was one of the first reported in the US in 2024. His cousin, Lorelei Walker, detailed the extent of his loss to DailyMail.com. Ian was the second member of his family affected by this disease.
She told DailyMail.com: ‘Ian is the second in my family to succumb to this illness. If I hadn’t gone through this with my husband, I would never have known what this disease is and the damage it causes, not only to the person fighting it but to the families and friends who watch it.’
Lurking in moist soil, leaves and rotting wood, the fungi release spores into the air when disturbed, which can embed themselves in tissues and cause infections. The fungus that causes blastomycosis, for example, transforms into a type of yeast that replicates in the lungs and causes infection.
Mrs Walker does not know to this day how her husband Ira, who had underlying kidney disease, became infected in June 2020. At the height of the global Covid pandemic, Ira was rushed from his dialysis session in an ambulance to the hospital in June 2020. after weeks of shortness of breath, fatigue and muscle aches.
An X-ray revealed opaque masses in his lungs that suggested to doctors that he had pneumonia, although his condition did not improve with standard treatment for lung infection.
He was admitted to the hospital and subsequent tests confirmed blastomycosis.
The diagnosis of blastomycosis requires chest x-rays or CT scans to detect lung masses or cavities. Doctors usually also take fluid or tissue samples to look for evidence of yeast cells that Blastomyces transforms into when they invade the lungs.
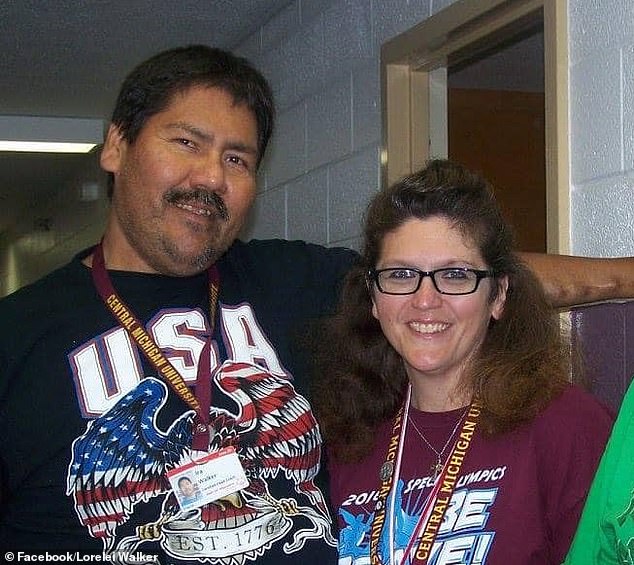
Ira Walker, pictured left, succumbed to blastomycosis in 2020. His wife Lorelei, right, told DailyMail.com she still doesn’t know how he got sick.

Ira’s immune system was not strong at first. He had been on dialysis when he was rushed to the hospital and eventually diagnosed with blastomycosis.
Ira languished in a hospital for a month after doctors surgically cut an opening from his neck to his windpipe, before being transferred to a specialized facility to receive a higher level of care. While the hope was for him to regain his lost strength and muscle mass, his situation only got worse.
She told DailyMail.com: ‘Instead of regaining his strength, he became weaker. Every time the hospital called, there was news of another setback.
‘At the end of September, I received a call from her sister telling me that she had made the decision to return home for palliative care.
‘He put the phone to his ear so I could talk to him and confirm it. A few days later, I spoke to his case manager and made arrangements for him to come home.’
Studies have shown that a warming climate creates exceptionally hospitable environments for many types of the most sinister fungi and may even help them mutate in such a way that they cannot be treated with standard medications.
The fungus that causes valley fever, coccidioides, thrives in hot desert environments, becoming increasingly hot and dry. And another, Histoplasma, which causes histoplasmosis, thrives in the moist soil of the East Coast, where it rains more and more as the years go by.
With a changing environment allowing fungi to constantly thrive and adapt, there are concerns that the current arsenal of antifungal treatments will fail, leaving healthcare workers to deal with a growing crisis of untreatable pathogens.
Neither Mrs Walker nor the Pritchard family can say where their loved ones were exposed, but it could have been anywhere outdoors, given that Blastomyces thrives in moist soil and environments.
The Midwest has gotten warmer and storms are getting more intense. Annual rainfall has increased by up to 20 percent in some areas of the region since 1900.
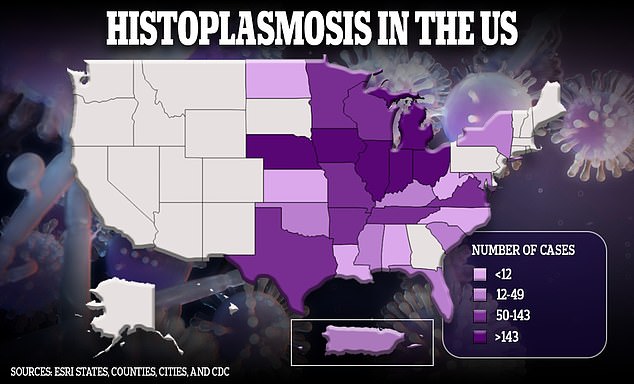
Average winter temperatures in the U.S. have increased nearly three degrees and spring temperatures have increased approximately two degrees. Warmer climates bring a longer growing season for fungi, allowing them to thrive for longer periods and reproduce more widely.
Fungi are also increasingly able to migrate to new environments that were inhospitable decades ago. Vermont, which is not a state where Blastomyces is considered endemic, has become the fungus’ newest home.
Earlier this year, Vermont health officials and the Centers for Disease Control and Prevention reviewed insurance claims records to find cases of blastomycosis, which the state is not required to report.
they discovered 114 residents who had the infection. Of those 114 diagnoses, 30 had one or more blastomycosis-related hospitalizations and four died from the infection.
Massachusetts also does not have to report blastomycosis cases to the federal government. It was there that Darcy Coderre, 60, became seriously ill with what his doctors originally deduced was pneumonia.
They also believed the mark on his lung was cancer when he first presented to doctors in 2016. Only after performing a biopsy did doctors realize they were actually dealing with a case of blastomycosis.
She said: ‘My doctor was a bit surprised. He said he hadn’t seen any cases of that in Massachusetts.
‘We tried to find out where I got it from and we couldn’t find out. I garden, so we thought it might have been from the soil. I go out for walks, but I pretty much stay on the trails.
The antifungal medications worked and he recovered, but he still has two scars on his lungs from the infection. She now also has asthma, which she believes is a lingering effect of her illness.
Another sinister fungus is on the rise, but its links to climate change are murkier. Instead, the Candida auris strain is more associated with hospital settings where it can spread quickly, especially among residents of long-term care facilities or among people with indwelling devices (such as catheters, tracheostomies, or wound drains) or mechanical ventilators.
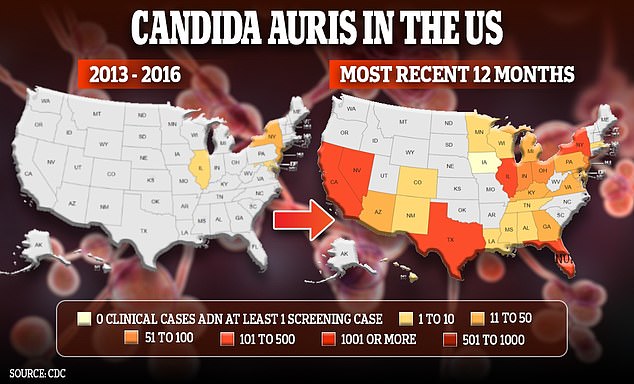
Candida auris is a serious global health concern and is becoming more common in the US with each passing year.
Tracking by the federal government shows about 60 infections in the US between 2013 and 2016, but there were more than 2,300 cases in 2022 alone.
Antifungal medications may also be ineffective. Some C. auris infections have been resistant to all three types of antifungal medications: azoles, echinocandins, and amphotericin B. Echinocandins are the first line of treatment to treat C. auris.
Multidrug-resistant strains of C. auris have become more common in recent years.